This week’s health news roundup contains stories regarding multiple sclerosis, testosterone and type 2 diabetes, Crohn’s disease, rheumatoid arthritis and psoriasis and psoriatic arthritis. This week we took a closer look at smoking and multiple sclerosis progression, testosterones role in blood sugar regulation, IBD and creeping fat, rheumatoid arthritis increasing with workload and biologics to treat psoriasis and psoriatic arthritis can help lower depression.
In case you missed any of these latest health news articles we have compiled them together for you for quick reference.
 Multiple sclerosis (MS) progression increases with continued smoking after diagnosis: Study
Multiple sclerosis (MS) progression increases with continued smoking after diagnosis: Study
Advertisement
Multiple sclerosis (MS) progression increases with continued smoking after diagnosis, according to research. Compared to multiple sclerosis patients who quit after diagnosis, those who continue smoking have worse outcomes and greater progression of the disease.
Smoking is a known risk factor for multiple sclerosis. The researchers looked at 728 smokers: 332 were considered continued smokers – meaning they continued smoking the year after diagnosis – and 118 were quitters who stopped smoking the year after diagnosis. The researchers also included data on 1,012 patients who never smoked.
The analysis revealed that after each additional year of smoking, disease progression accelerated by 4.7 percent. Disease progression was also found to be faster in continued smokers, compared to those who quit.
The study concluded, “This study demonstrates that smoking after MS diagnosis has a negative impact on the progression of the disease, whereas reduced smoking may improve patient quality of life, with more years before the development of SP [secondary progressive] disease. Accordingly, evidence clearly supports advising patients with MS who smoke to quit. Health care services for patients with MS should be organized to support such a lifestyle change.” Continue reading…
 Testosterone helps regulate blood sugar, low testosterone raises type 2 diabetes risk in men: Study
Testosterone helps regulate blood sugar, low testosterone raises type 2 diabetes risk in men: Study
Low testosterone raises the risk of type 2 diabetes in men as testosterone helps regulate blood sugar levels. The researchers found that testosterone triggers essential signaling mechanisms in islets, which are clusters of cells within the pancreas producing insulin.
Senior author Dr. Franck Mauvais-Jarvis said, “We have found the cause — and a potential treatment pathway — for type 2 diabetes in testosterone-deficient men. Our study shows that testosterone is an antidiabetic hormone in men. If we can modulate its action without side effects, it is a therapeutic avenue for type 2 diabetes.”
For the study, researchers used specifically bred male mice with pancreatic beta cells lacking the receptor to testosterone. The mice were fed a typical Western diet rich in sugars and fat, and then tested their response to glucose. The mice lacking the androgen receptors developed lower insulin secretion, which led to glucose intolerance, compared to control mice.
The study suggests that testosterone amplifies the islet impact of glucagon-like peptide-1 (GLP-1), a hormone produced after a meal, which is currently used as a diabetes treatment. Continue reading…
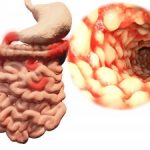 Crohn’s disease, ulcerative colitis progression and development linked to “creeping fat”: Study
Crohn’s disease, ulcerative colitis progression and development linked to “creeping fat”: Study
Crohn’s disease and ulcerative colitis progression and development have been found to be linked to “creeping fat.” Researcher Charalabos Pothoulakis said, “A well-appreciated feature of IBD [inflammatory bowel disease], especially longstanding Crohn’s disease, is intra-abdominal fat, also known as ‘creeping fat,’ which wraps around the intestine. However, it’s not clear whether this fat is protective or harmful. Our study offers insight into this phenomenon. We found that intra-abdominal fat cells may normally be programmed to dampen inflammation but, in fact, have acquired a tendency to promote inflammation in IBD.”
The researchers collected mesenteric fat tissues from 11 colitis patients, 11 Crohn’s patients, and 10 non-IBD controls. The researchers then isolated and cultured preadipocytes, cells that differentiate into becoming part pf adipose tissue where fat is stored for energy. They intended to evaluate the effect of the neuropeptide substance P on the expression of cytokines, which are small proteins important for cell signaling.
The researchers found that signaling mediators produced by the intra-abdominal fat cells in the controls were significantly different from those in the IBD patients. This indicates that these cells are actively involved in gut immunity and inflammation, as pointed out in the press release.
Increased expression of neurokinin-1 and neurokinin-2 receptor mRNA was observed in IBD preadipocytes – compared to controls, while increased expression of substance P mRNA was observed in ulcerative colitis preadipocytes – compared to Crohn’s patients and controls.
The researchers wrote, “Fat represents a novel reserve of IL-17 during the disease and may affect the progress of IBD by altering intestinal responses via interactions with IL-17RA. This observation along with the identification of IL-17 as the most consistently regulated mediator in human mesenteric preadipocytes isolated from IBD patients in response to [substance P] suggests a potential role for this neuropeptide in the regulation of inflammatory changes in the intestine during IBD (both ulcerative colitis and Crohn’s disease) via modulation of IL-17 expression in the adjacent mesenteric preadipocytes. Furthermore, our observations introduce the preadipocytes as a novel cellular population with immune properties that are likely involved in the regulation of intestinal inflammation during IBD.” Continue reading…
 Rheumatoid arthritis risk increases with repetitive physical workload: Study
Rheumatoid arthritis risk increases with repetitive physical workload: Study
Rheumatoid arthritis (RA) risk increases with repetitive physical workload, according to research. Previously, prolonged work-related physical activity has been linked to osteoarthritis in some joints.
For the study, the researchers looked at self-reported information from 3,680 rheumatoid arthritis patients along with 5,935 controls.
Miss Pingling Zeng of the Institute of Environmental Medicine said, “We found that some types of physical workload increased the odds of developing RA more than others. There also appeared to be a significant interaction between genetic makeup, in terms of HLA-DRB1 genes, and the risk of ACPA-positive RA from specific types of physical workload.”
The estimated odds ratio of developing rheumatoid arthritis in participants exposed to the repetitive workload vs. unexposed participants was equal to or greater than 1.5. Certain types of manual labor were at an increased risk – for example, in construction industry, manual work above the shoulder level or below the knee level in construction.
Miss Zeng concluded, “These new insights into the cause of RA may hopefully lead to effective strategies to prevent the development of RA, particularly in those RA patients with a susceptible genotype.” Continue reading…
 Psoriasis and psoriatic arthritis patients receiving biologics therapy show reduction in depression and insomnia: Study
Psoriasis and psoriatic arthritis patients receiving biologics therapy show reduction in depression and insomnia: Study
Psoriasis and psoriatic arthritis patients receiving biologics therapy show reduction in depression and insomnia. The National Psoriasis Foundation states that individuals affected by psoriasis or psoriatic arthritis are at a higher risk of depression, compared to the general public. Symptoms of depression include insomnia and anxiety, which causes patients to use high amounts of antidepressants.
The researchers identified 980 patients with psoriasis or psoriatic arthritis receiving biologics therapy. The researchers compared rates of patients taking medications for depression and insomnia before and after biologics therapy.
Prior to biologics treatment, 20 percent of patients were taking antidepressants. After two years of biologics, there was over a 40 percent reduction in antidepressant use.
Advertisement
The researchers also found that being over the age of 45, being a woman, having comorbidities, and suffering from psoriatic arthritis are independent risk factors for depression and insomnia.
Biologics therapy in those younger than 45 actually sped up the reduction of the antidepressant use.
The authors concluded, “The results suggest that biologics therapy may be associated with reduced rates of depression and insomnia, and a reduced rate of regular antidepressant use in psoriasis patients.” Continue reading…
