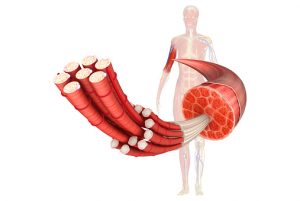
 Myofibrillar myopathy is a muscular disease and part of a group of disorders called muscular dystrophies. The condition is characterized by improper functioning of muscle fibers causing weakness of skeletal muscles. This can affect muscles involved in movement and in some cases even the muscles of the heart.
Myofibrillar myopathy is a muscular disease and part of a group of disorders called muscular dystrophies. The condition is characterized by improper functioning of muscle fibers causing weakness of skeletal muscles. This can affect muscles involved in movement and in some cases even the muscles of the heart.
This condition is different from other muscular neuropathies that are primarily caused by problems involving nerves of the central nervous system. Instead, myofibrillar myopathy stems from a problem of the products that make up muscle fibers themselves.
What causes myofibrillar myopathy?
Advertisement
Myofibrillar myopathy is primarily thought to be caused by a genetic mutation of genes responsible for making the proteins in muscle fibers strong. Specifically, the genes that encode the linking of muscle units called sarcomeres become dysfunctional, leading to muscle weakness. These links are responsible for joining together so that muscles are strong enough to help our body move.
Additionally, some think that the condition may be also caused by poor diet and stress, which leads some to emphasize the implementation of a proper healthy diet to help circumvent some of the symptoms of the condition. However, more research is needed as myofibrillar myopathy is a rare disorder.
What are the symptoms of myofibrillar myopathy?
Myofibrillar myopathy symptoms vary from patient to patient, with affected individuals commonly developing cramps and muscle weakness in mid-adulthood. However, there are cases where features of the condition appear anytime between infancy and late adulthood.
Muscle weakness is commonly seen in the hands and feet, also known as the distal muscles. This may cause individuals to have a hard time holding an object in their hand or even suffer from repeated falls due to weakness of the leg and calf muscles. Muscle weakness throughout the body also occurs and may present as facial muscle weakness, which can cause swallowing and speech difficulties. Muscle weakness is known to worsen over time.
Another one of myofibrillar myopathy complications involves the muscles of the heart (cardiomyopathy), muscle pain (myalgia), loss of sensation and weakness in the limbs (peripheral neuropathy), and even respiratory failure. Skeletal problems include scoliosis (abnormal curvature of the spine), contractures (joint stiffness), and clouding of the lens of the eye (cataracts).
Diagnosis of myofibrillar myopathy
Developing abnormal muscle weakness is one of the most important signs that your doctor will identify that prompts further investigation. Having an additional complication, such as cardiomyopathy, will help narrow down the possible causes of the condition. Additionally, a complete family history of known relatives with similar traits of muscle weakness or cause of death will signify a genetic link.
The following are some diagnostic tests that can help in the diagnosis of myofibrillar myopathy:
- Electromyography: Measures the response of muscles to an electrical stimulus.
- Muscle biopsy: Taking a piece of muscle tissue and looking at it under a microscope for characteristic findings.
- Creatine kinase test: An enzyme found in the blood that can provide information about the health of the muscles.
- Genetic testing: Looking for specific genes associated with myofibrillar myopathy. Can confirm the diagnosis and provided information about prognosis of the particular mutation found.
Related: How to treat ischemic cardiomyopathy? Causes, symptoms, and prognosis
Treatment and prevention of myofibrillar myopathy
Treatment will depend on the signs and symptoms currently affecting the patient and focuses on strengthening muscle power in an attempt to improve quality of life. This often comes in the form of physical therapy, as the patient performs various exercises to improve muscle movement and strength. Braces and other assistive devices may also be implemented to help prevent damage from falls and injury.
Specific complications, such as cardiomyopathy, may improve with a pacemaker and implantable cardioverter defibrillator (ICD). Life-threatening cardiomyopathy may even require a heart transplant.
If the breathing muscles become involved, the use of respiratory support devices initially at night and later in the day can help prevent respiratory failure.
Because the condition can vary greatly among patients, there is no single best treatment for myofibrillar myopathy. If you or a close family member has been diagnosed with the condition, obtaining genetic counseling for yourself and learning how it may affect your own offspring is in your best interest.
Advertisement
Related:
20 essential oils for muscle pain and how to use them
Muscle fatigue: Causes, symptoms, and treatment
