
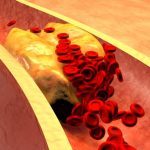
Peripheral vascular disease (PVD) occurs when blood can’t get to where it needs to go due to a narrowing of blood vessels. This can be the result of atherosclerosis, where plaque build-up causes the arteries to become narrow and harder. As plaque continues to build-up, it can result in a blockage of the artery that leads to organ damage or loss of limbs if untreated.
Advertisement
The body uses the circulatory system—which relies on veins, arteries, and capillaries—to carry blood throughout the body. Arteries carry oxygenated blood away from the heart to organs and cells. Veins transport oxygen-depleted blood through the kidneys, lungs, and liver where it is filtered and returned to the heart. While there are exceptions, the direction of blood flow is what distinguishes arteries and veins from each other.
PVD may be referred to as several different other names including arteriosclerosis obliterans, arterial insufficiency of the legs, claudication, and intermittent claudication.
Two types of peripheral vascular disease
Peripheral vascular disease (PVD) refers to diseases of the blood vessels outside of the heart and brain. When veins and arteries narrow and limit blood flow, this is part of PVD. In both PVD and PAD, the arteries continue to narrow over time, which limits circulation. Other conditions related to PVD include deep vein thrombosis (DVT), varicose veins, and chronic venous insufficiency. Lymphedema is an example of PVD that affects the lymphatic vessels.
Peripheral Artery Disease:
Here are some other conditions related to peripheral artery disease:
Raynaud’s disease: This is a condition in which, during times of stress or in response to cold temperature, the blood vessels in the hand narrow or spasm, restricting blood flow. This is often seen as blue discoloration of the fingertips. The sensation of coldness, numbness, and tingling may also be present. Raynaud’s symptoms may also be seen in other distant parts of the body, such as the nose or toes.
Atherosclerosis: Here, blood vessels narrow due to cholesterol plaque buildup on the walls of your arteries, eventually restricting blood flow. This means greater force is required for blood to pass through these narrow areas to be able to deliver adequate blood supply, causing increased blood pressure. If this blood vessel narrowing occurs in the vessels supplying the heart, it can trigger a heart attack.
Buerger’s Disease: A chronic inflammatory disease in the peripheral arteries and extremities which can cause clots in the legs that can eventually lead to a blockage. Buerger’s disease most commonly occurs in men aged 20 to 40 who are smokers. Symptoms include pain in the legs or feet, clammy cool skin, and a diminished sense of heat or cold.
Peripheral Venous Disease:
Here are some examples of peripheral venous diseases:
Thrombophlebitis: This inflammatory process causes the development of blood clots that block one or more veins. The legs are usually the most common extremity involved. Superficial thrombophlebitis often appears as redness and swelling in the affected area. If the condition occurs deeper beneath the skin, it may trigger a condition called deep vein thrombosis.
Chronic venous insufficiency: This condition is characterized by pooling blood in the lower extremities, as it has become difficult for the blood vessels to return blood to the heart. Chronic venous insufficiency can be the result of obesity, a history of varicose veins, deep vein thrombosis, sedentary lifestyle, long periods of sitting or standing, being over 50 years old, being female, or being pregnant. Symptoms often include swelling in the lower legs or ankles, aching feeling in the legs, and development of varicose veins.
Varicose veins: Varicose veins are visible veins that may look dark purple or blue in color, usually in the legs and feet. These enlarged and discolored veins may not pose any immediate health concerns to some patients and can be more of a cosmetic problem, looking unsightly or unattractive. However, some individuals experience aching pain and discomfort and this could signal a higher risk for other circulatory problems. Varicose veins are thought to be a result of prolonged standing or walking that increases the pressure in the veins of the lower body, with the effects of gravity mostly to blame. Dysfunction of tiny valves in the blood vessels themselves have also been seen to play a role. Other risk factors include age, sex, family history, and obesity.
There are two types of peripheral vascular disease:
1. Functional PVD: There are no defects in the blood vessels themselves. Typically, functional PVD is due to spasms, which can come and go, or factors such as working with machinery that vibrates, cold temperatures and smoking.
2. Organic PVD: Organic PVD refers to structural changes in the blood vessels. Inflammation and tissue damage are examples of organic PVD. Peripheral artery disease in particular occurs when fatty plaques build up in the arteries and limit blood flow.
Causes and complications of PVD
 Both functional PVD and organic PVD can be caused by smoking. Causes of functional PVD, which differ from organic PVD include emotional stress, cold temperatures and operating vibrating machinery.
Both functional PVD and organic PVD can be caused by smoking. Causes of functional PVD, which differ from organic PVD include emotional stress, cold temperatures and operating vibrating machinery.
Organic PVD may be caused by fatty build-up in the arteries as seen with high cholesterol, high blood pressure, infection, injury to extremities, coronary heart disease and diabetes.
Complications of PVD include amputations, heart attack, poor wound healing, restricted mobility due to pain and discomfort, severe pain in the affected area, and three times higher risk of stroke.
What are the symptoms of peripheral vascular disease?
Early symptoms of peripheral vascular disease:
- Painful cramping
- Aches
- Fatigue
- Burning sensations.
Severe symptoms of peripheral vascular disease:
- Changes to skin – color, thinning etc.
- Weak pulse in leg and feet
- Gangrene – tissue death caused by lack of blood flow
- Wounds won’t heal
- Reduced hair growth on legs
- Toes may turn blue due to lack of oxygenated blood
- Burning sensation in toes
- Leg cramps while in bed
- Muscles feel numb or heavy
- Limbs may appear red or blue
- Toenails become thick and opaque.
Many of these symptoms may be confused with aging. If you start to notice these changes speak with your doctor.
Risk factors of peripheral vascular disease
 Medical and lifestyle factors may increase one’s risk of developing peripheral vascular disease, these include:
Medical and lifestyle factors may increase one’s risk of developing peripheral vascular disease, these include:
- High or abnormal cholesterol
- Cerebrovascular disease (stroke)
- Cardiovascular disease
- Diabetes
- Family history of cholesterol, blood pressure or PVD
- Hypertension
- Kidney disease
- Being overweight
- Smoking
- Lack of engagement of physical activity
- Being over the age of 50.
How to diagnose peripheral vascular disease
Peripheral vascular disease is diagnosed with a variety of exams and tests. First and foremost, your doctor will try to rule out other causes for your symptoms. They might start with a questionnaire that includes a series of six questions and a pain diagram. This is known as the Edinburgh Claudication Questionnaire and it is 90 percent effective at diagnosing PVD.
Another widely used test is known as ankle/branchial index (ABI), which compares the blood pressure in the arm with the blood pressure in the legs. In a healthy person, the blood pressure will be higher in the arms. Someone with PVD will have higher blood pressure in the legs.
Your doctor may also recommend a treadmill exercise test, which is usually a follow-up to the ABI. Blood pressure of the arms and legs are taken prior to exercise and again after exercise on the treadmill. A significant drop in blood pressure post exercise indicates PVD.
A special x-ray, known as angiography or arteriography, may be used, which injects a colored dye into the arteries to highlight narrow or blocked arteries. Due to its invasive nature, doctors may skip this type of x-ray and opt for an MRI scan instead.
 How to treat PVD
How to treat PVD
Medical treatments for PVD include percutaneous balloon angioplasty. This technique enlarges the artery using a balloon to help open up the artery without the use of surgery. The angioplasty is conducted by inserting a catheter into the affected artery. A tiny balloon is then attached to the end and inflated to push aside plaque and widen the artery so that blood flow is no longer restricted. The balloon is then deflated and removed from the artery.
Advertisement
Your doctor may also recommend medications such as antiplatelets that make blood platelets less likely to stick together, which can increase the risk of a clot. Anticoagulant medications prevent blood clots by thinning the blood. They may also recommend cholesterol-lowering drugs, as cholesterol can contribute to more plaque build-up.
Home remedies and prevention of peripheral vascular disease
One way to treat and prevent peripheral vascular disease is by changing lifestyle habits. This includes cessation of smoking, achieving a healthy weight, managing diabetes, lowering cholesterol (this can be done through diet and exercise), managing hypertension, and eating well.
Ensure that you follow your doctor’s recommendations to treat PVD—both medically and lifestyle changes—to reduce your risk of complications resulting from peripheral vascular disease.
