 Acute coronary syndrome does not describe one specific medical condition. It’s associated with any sudden reduction of the blood flow to the heart. One condition that falls under the category of acute coronary syndrome is a heart attack, where cell death occurs and causes damage to the heart tissue. Even if cellular death does not occur due to acute coronary syndrome, the reduced blood flow to the heart can cause permanent damage and an increased risk of heart attack. Acute coronary syndrome is considered a medical emergency.
Acute coronary syndrome does not describe one specific medical condition. It’s associated with any sudden reduction of the blood flow to the heart. One condition that falls under the category of acute coronary syndrome is a heart attack, where cell death occurs and causes damage to the heart tissue. Even if cellular death does not occur due to acute coronary syndrome, the reduced blood flow to the heart can cause permanent damage and an increased risk of heart attack. Acute coronary syndrome is considered a medical emergency.
What Are the Various Types of Acute Coronary Syndrome?
There are three types of conditions that fall under the umbrella of acute coronary syndrome.
Advertisement
Unstable angina is a medical condition where the heart does not receive enough blood. It usually occurs while resting and can result in a ruptured blood vessel.
Non-ST-segment elevation myocardial infarction or heart attack (NSTEMI) is a form of heart attack. It is the less common form of heart attack and usually does not cause nearly as much damage. This type of heart attack usually forms due to a partial blockage of the coronary artery.
ST-segment elevation myocardial infarction or heart attack (STEMI) is the most common type of heart attack, causing the most damage to the heart and its tissues. In an electrocardiogram, STEMI will demonstrate elevated ST wave, progression to Q wave, and the full blockage of a coronary artery, which is how it is differentiated from NSTEMI heart attack.
What Are the Causes and Risk Factors for Acute Coronary Syndrome?
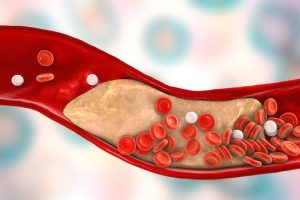
Acute coronary syndrome is generally caused by the build-up of fatty deposits (plaque) in the veins and arteries leading into the heart, more specifically the coronary arteries. When plaque develops on the walls of the arteries, there is an increased risk that it can break off, causing the blood vessel to rupture or forming a clot within the vessel. This causes the decreased or blocked flow of blood to the heart. If the arteries become too narrow due to the build-up of plaque, blood flow can also become significantly decreased, even without a clot.
The risk factors for acute coronary syndrome are similar to those for other coronary diseases. These include:
- Old age, above 45 for men and 55 for women
- High blood pressure
- High cholesterol
- Smoking
- Sedentary lifestyle
- Unhealthy diet
- Obesity or being overweight
- Diabetes
- Family history of chest pain, coronary diseases, or stroke
- For women, a history of high blood pressure, preeclampsia, or diabetes specifically during pregnancy
Acute Coronary Syndrome Symptoms
If the flow of oxygen through the bloodstream into the heart becomes too depleted, the cells in the heart will die, causing damage to the tissues. The symptoms of acute coronary syndrome generally occur very suddenly but can continue on and off progressively after the initial onset. The most common symptom, as with other coronary diseases, is chest pain or discomfort. It is often described as aching, intense pressure, tightness, or burning. Women, older patients, and patients with diabetes are often found to have acute coronary syndrome without experiencing chest pain or discomfort. If you fall into one of these categories, be aware of the additional symptoms that can occur with acute coronary syndrome.
Other acute coronary syndrome symptoms include:
- Pain from the chest radiating into the shoulders, arms, upper abdomen, back, neck or jaw
- Nausea or vomiting
- Indigestion
- Shortness of breath
- Sudden, heavy sweating
- Lightheadedness, dizziness, or fainting
- Unusual or unexplained fatigue
- Feeling restless or apprehensive
How to Diagnose Acute Coronary Syndrome
As acute coronary syndrome is a medical emergency, you should go to the hospital immediately if you are concerned that you may be suffering from this medical condition. While in the emergency room, a doctor will confirm all your symptoms and ask you questions to assess your family history.
Tests used to diagnose acute coronary syndrome include:
- Electrocardiogram (ECG) measures electrical activity in the heart through electrodes that are attached to your skin. Abnormal or irregular impulses can indicate poor heart function, due to a lack of oxygen to the heart. Certain patterns in the electrical signals could also indicate the general location of a potential blockage.
- Blood tests can detect certain enzymes that are produced in the case of cell death.
- Coronary angiogram uses x-ray imaging to see the blood vessels in the heart. A catheter is threaded through an artery, usually in the arm or groin, into the arteries in your heart. A dye is injected into the tube into the arteries. Using x-rays, the blockage can be revealed in the arteries.
- Echocardiogram uses sound waves, directed at your heart from a wand-like device, to produce a live image of your heart. An echocardiogram can help determine whether the heart is pumping correctly.
- Myocardial perfusion imaging (MPI) shows how well blood is flowing through your heart. A very small amount of radioactive substance is injected into the blood and a specialized camera is used to detect the blood as it moves through the heart to reveal whether there is enough blood flow through the heart muscles. The test can also reveal where blood flow is reduced.
- Computerized tomography (CT) angiogram uses x-ray technology and can produce multiple images of the heart, which can detect narrowed or blocked coronary arteries.
- Cardiac perfusion scan can detect if the heart is receiving enough blood and areas where there may be damage to the heart.
Acute Coronary Syndrome Treatment
Treatment of acute coronary syndrome focuses on relieving the immediate pain a patient is in as well as clearing the arteries of blockages, which may be reducing blood flow. In the long-term, patients may need therapies and treatments to improve heart function after the damage of a heart attack.
Medications prescribed focus on clearing the arteries of blood clots, lowering blood pressure and cholesterol, improving overall circulation, and relaxation of the heart muscles.
In some cases, patients may require surgery to repair the arteries or to prevent them from narrowing further.
Acute Coronary Syndrome Home Remedies
Aside from medication, implementing simple lifestyle changes and home remedies can greatly reduce the effects and risk of developing acute coronary syndrome.
Advertisement
Recommended lifestyle changes include:
- Quit smoking
- Maintain a healthy diet
- Exercise regularly
- Keep an eye on your blood pressure and cholesterol
- Maintain a healthy weight
- Drink in moderation or not at all
- Manage stress
Acute coronary syndrome is an umbrella term that describes the cause of several coronary conditions. Acute coronary syndrome occurs when there is a sudden reduction in the blood flow to the heart. This can be caused by the build-up of fatty deposits in the coronary arteries, which then rupture or break off and cause blood clots in the blood vessels, cutting off oxygen and blood supply to the heart. When this happens, the cells in the heart could die, resulting in heart tissue damage and heart attack. Maintaining a healthy lifestyle can greatly reduce the risk of developing acute coronary syndrome.
Related: Costochondritis: Common cause of chest pain, can mimic a heart attack and other heart conditions
