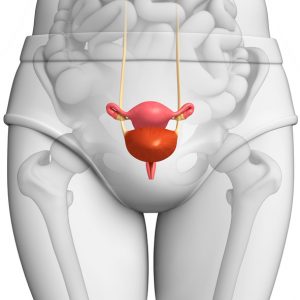
A prolapsed bladder can be categorized into one of the following grades: mild, moderate, severe, and complete. In a mild grade, only a small portion of the bladder falls into the vagina. In moderate, the bladder drops enough to be felt at the opening of the vagina. In severe, the bladder begins to protrude through the vaginal opening, and in complete, the entire bladder protrudes out of the vagina. This last stage is often associated with other forms of organ prolapse.
Causes and symptoms of bladder prolapse
The most common cause of bladder prolapse is aging. The muscles that support the bladder become weaker over time, especially when women enter menopause. This is associated with a reduced production of estrogen, which is responsible for keeping the muscles strong.
Childbirth can also cause bladder prolapse with stress to the vaginal tissues and supporting muscles.
Lastly, straining caused by heavy lifting, bowel movements, or long-term coughing or constipation can also weaken the muscles, thus contributing to a prolapsed bladder.
Signs and symptoms of a prolapsed bladder include:
- Frequent urination or a strong urge to urinate
- Incontinence
- Not feeling relief even after urinating
- Frequent urinary tract infections
- Pain in the vagina, pelvis, lower abdomen, or groin
- Heaviness or pressure in the vaginal area
- Pain during sexual intercourse
- Tender or bleeding tissue sticking out of the vagina
Tests and diagnosis for prolapsed bladder
Your doctor may also test your nerves, muscles, and the intensity of the urine stream. Other tests include urodynamics and a cystoscopy to look inside the bladder.
Treatment options for bladder prolapse
There are other, less intrusive modes of treatment for a prolapsed bladder. One of the options is not taking any course of treatment at all if there are no symptoms present. Other forms of treatment include behavior therapy, Kegel exercises, pelvic floor physical therapy, use of a vaginal support device, or drug therapy, which may involve estrogen replacement.
Surgery is another option for a prolapsed bladder. Surgery options include open surgery, minimally invasive surgery, laparoscopic surgery, and robot-assisted laparoscopic surgery.
The goal of the surgery is to repair any damaged muscles or tissue, and augment the bladder with a surgical material.
Prolapsed bladder prevention and management
Keeping a healthy weight is also important because obesity puts added stress onto the pelvic muscles, further increasing the risk of a bladder prolapse.
It’s important to know when to see your doctor for a prolapsed bladder in order to prevent complications.
When to call a doctor for bladder prolapse
You should see your doctor as soon as you start spotting any symptoms of a prolapsed bladder. Often, cystocele is associated with a prolapse of other pelvic organs, so there may be other complications underway as well.
The sooner you see your doctor with regards to your prolapsed bladder, the earlier the treatment can begin before the condition worsens.