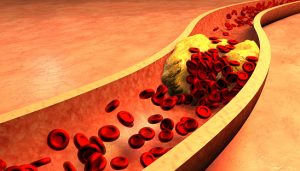
If cellular tissue is devoid of oxygen for a long period of time, it will lead to tissue damage and cell death in the affected area. Arterial blood clots are considered a medical emergency and require immediate attention.
A blood clot (thrombus) not only restricts blood flow, but also has the potential to break apart, forming emboli; a free-floating blood clot with the potential to block blood supply elsewhere.
What are the causes and risk factors of an arterial embolism?
The formation of a blood clot within tends to begin with blood vessel damage. When this occurs, the body attempts to try and repair this damage by recruiting various coagulation factors and constituents that temporarily cover the damaged area so the process of healing can occur. However, in some cases, these coagulation products may accumulate in excess, causing them to impede blood flow.
Blood clots can also be created in the heart in cases of cardiac arrhythmia. In this scenario, the heart does not beat in its normal rhythmic fashion, which causes blood to pool in one of its chambers. When this occurs, blood will begin to coagulate, forming a blood clot. The most worrisome complication with blood clots is their potential to travel to the brain or the heart, causing a stroke or heart attack, respectively.
A condition called atherosclerosis is also a major cause of blood clot (thrombus) formation due to an accumulation of cholesterol plaques lining blood vessels. When significant plaque accumulation occurs, especially in the blood vessels that supply the heart muscles, blood cannot circulate efficiently due to impaired expansion and contraction of the blood vessels. The most worrisome issue, however, is the sudden formation of a thrombus or blood clot at atherosclerotic choke points. When this occurs in the heart vessels, a heart attack will shortly ensue.
There are also many genetic conditions that increase the risk of blood clot development such as factor V Leiden deficiency, protein S deficiency, and protein C deficiency. There also exist several medications that can promote a clotting environment.
Risk factors for arterial embolism develop include:
- High blood pressure
- Diabetes
- Increased blood lipids – high LDL, low HDL
- Tobacco smoking
- Sedentary lifestyle
- Obesity
- Getting older
- Increased platelet counts
- Patent foramen ovale – a congenital heart condition
- Atrial fibrillation
- Mitral stenosis – related to rheumatic fever and endocarditis
- Heart disease
- Recent surgery
Arterial embolism symptoms
Arterial embolism symptoms will vary depending on the area of the body they affect. Symptoms may begin quickly or slowly depending on the size of the obstruction and how much blood flow is blocked. Common symptoms of an arterial embolism in the body tend to involve pain and a temporary decrease in organ function. The following are some more specific symptoms depending on the affected region.
Arterial embolism signs and symptoms are dependent upon the location. These may include:
- Embolism in the limbs: Weakness, cramps, change in skin color, feeling of numbness and tingling sensation, and pain in the affected area.
- Embolism in the coronary artery of the heart: Chest pain, nausea, vomiting, sweating, pain radiating to the left arm associated with anxiety.
- Embolus in the brain: Temporary or permanent loss of function pertaining to the region of the brain affected. This may include the ability to move, think, speak, and touch.
- Embolus in abdominal blood vessels: Abdominal pain after meals that resolves in a few hours.
How to diagnose arterial embolism?
Once the symptoms of a potential arterial embolism are documented, additional tests will be ordered to provide evidence that a blood clot did occur. This will allow physicians to confidently use anticoagulation therapy and medication. The following are tests used to determine any underlying causes for thrombosis or embolism and to confirm any blood supply obstruction:
- Doppler ultrasound
- Echocardiography
- Transesophageal echocardiography (TEE)
- Arteriography
- Angiography
- Magnetic resonance imaging (MRI)
- Computed tomography (CT)
- Blood tests – looking for biomarkers of cell damage like cardiac enzymes
- Blood cultures
- Electrocardiography (ECG/EKG)
- Angioscopy
Diagnostic tests are used in conjunction with clinical presentation to reach a definitive diagnosis.
Treating arterial embolism
Treatment will involve controlling symptoms and improvement of blocked blood flow, with the hopes of fully restoring blood supply to the affected area. Arterial emboli are usually an emergency situation and require immediate treatment, as the chances of success decrease the longer you wait.
Medications include:
- Anticoagulants: Includes warfarin and heparin.
- Antiplatelet: Includes aspirin and clopidogrel.
- Thrombolytics: Such as streptokinase.
- Painkillers.
- Vasodilators.
Surgical procedures include:
- Arterial bypass: Creates a second source of blood supply to the affected region.
- Embolectomy: Directly removes the clot.
- Angioplasty: Done via balloon catheterization with or without stent placement.
Can arterial embolism be prevented?
Living a healthy lifestyle and stopping bad habits that affect your health will be the best form of prevention of arterial emboli. While this is true for the majority of people, there are some cases where the risk for arterial embolism development remains high, as seen in those with a genetic predisposition to blood clotting and those with uncontrol arrhythmias. If you are considered a high-risk patient, your doctor will likely prescribe a blood thinner or antiplatelet medication long term.
Complications of arterial embolism
- Myocardial infarction (heart attack)
- Transient ischemic attack (TIA)
- Stroke
- Tissue necrosis and gangrene
- Temporary or permanent decrease or loss of function
- Septic shock – seen in cases of septic embolism due to an infection
Prognosis of arterial embolism
The location of the arterial embolism will dictate how well the patient does after it occurs. The time it takes to receive treatment after the onset of blood clot symptom is paramount for improving prognosis, with sooner being better. Additionally, despite proper treatment and resolution of an arterial embolic attack, it can recur despite all efforts.
Related: Prediction and prevention of blood clots may be easier with new method