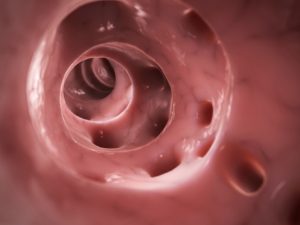
In inflammatory bowel disease (IBS), the innermost lining of the large intestine and rectum is affected. The symptoms of IBS develop gradually and can be life changing, making it difficult for some sufferers to maintain normal activities.
Ulcerative colitis vs. diverticulitis: Causes, symptoms, risk factors, and complications
Ulcerative colitis and diverticulitis are two conditions affecting the colon and gastrointestinal system. Nonetheless, their origins, symptoms, and treatments are quite different.
Ulcerative colitis is part of the group of conditions known as inflammatory bowel diseases (IBDs). Prior to the 20th century, before the rise of hygiene and urbanization, inflammatory bowel disease was quite rare. Currently, IBD is found in developed countries and is believed to be caused by a lack of germ resistance development – although the exact cause is still unknown.
The immune system in IBD patients mistakes food and bacteria in the gastrointestinal tract for an allergen or foreign substance, so it sends out cells to destroy the perceived enemy. The result of these attacks is chronic inflammation. Continue reading…
Blood in stool is a possible symptom for ulcerative colitis and Crohn’s disease. Blood in stool that is a result of an inflammatory bowel disease (IBD) will appear red or bright red, whereas if the blood is coming from the upper digestive tract, it will appear dark or even black.
Bleeding from the rectum is more common in ulcerative colitis than in Crohn’s disease, because colitis affects the rectum. Damage to the rectum and large intestine in ulcerative colitis explains the presence of blood in stool, as ulcers forming along the intestinal lining are bleeding. Continue reading…
Weight loss is quite common in ulcerative colitis, either due to loss of appetite or other factors. A type of inflammatory bowel disease (IBD), ulcerative colitis is often accompanied by painful flare-ups, so choosing the right foods to eat is often quite difficult.
Food plays a large role in ulcerative colitis because it can trigger a flare-up. Out of fear of feeling sick, some patients may avoid eating, cut down on their eating, or even lose their appetite altogether. All of these factors can result in unintended weight loss in ulcerative colitis patients.
Like many IBDs, ulcerative colitis may impact each person differently, so what may affect one patient may go unnoticed in the other. Although patients with ulcerative colitis may experience a host of differing symptoms, common ones include blood stools, bathroom urgency, loose stools, abdominal pain, worsening symptoms, inflammation, remission periods, and weight loss. Continue reading…
Ulcerative colitis and Crohn’s disease – both inflammatory bowel diseases (IBDs) – relapse risk varies during pregnancy, according to research. The study revealed that women with active IBD near the time of conception have a higher risk of a relapse during pregnancy. Furthermore, women with ulcerative colitis have a higher risk of IBD relapse, compared to women with Crohn’s disease.
Researchers from Erasmus MC-University Medical Center in Rotterdam wrote, “The effects of active disease on birth outcomes have been reported earlier, although these outcomes do not seem representative in the era of biologicals. Also, the retrospective nature of these studies makes it difficult to determine how these pregnant patients were treated for their disease flare.”
The researchers studied the effects of IBD on relapse during pregnancy and birth outcomes.
The researchers followed 298 pregnancies and 226 live births, measuring disease activity and assessing birth outcomes. Majority of women were advised to continue with their IBD treatment during pregnancy and 93 percent adhered to their treatment plan. The researchers wrote, “Periconceptional disease activity was defined as active disease…at any time from eight weeks before conception until the first two weeks of pregnancy.” Continue reading…
Ulcerative colitis causes fatigue and inflammation in the lining of the colon and rectum. Nearly 75 percent of inflammatory bowel disease (IBD) patients – including those with ulcerative colitis – experience fatigue during a flare-up.
A 2011 study also revealed that nearly 30 percent of participants had fatigue even when not experiencing a flare-up.
Although fatigue is not considered to be a universal symptom of ulcerative colitis, it is still reported to be quite common. A more effective management of ulcerative colitis may help you also experience greater improvements in energy levels.
Fatigue is much more than simply feeling tired. It can get so bad that it may actually impair one’s ability to carry out daily functions. The worse part about fatigue is its unpredictability. Fatigue can strike like lighting, turning a person from being full of life and energy to feeling completely wiped out.
In ulcerative colitis, fatigue may be your body’s response to inflammation in the colon. Fatigue could also be related to anemia, malabsorption of nutrients, side effects of medications, poor sleep, being overweight or underweight, and pain. Emotional stress could trigger fatigue, too. Continue reading…