 Lupus risk is associated with chronic exposure to staph (staphylococcus aureus) bacteria. A study from the Mayo Clinic revealed that chronic exposure to staph – even in small amounts – increases the risk of lupus.
Lupus risk is associated with chronic exposure to staph (staphylococcus aureus) bacteria. A study from the Mayo Clinic revealed that chronic exposure to staph – even in small amounts – increases the risk of lupus.
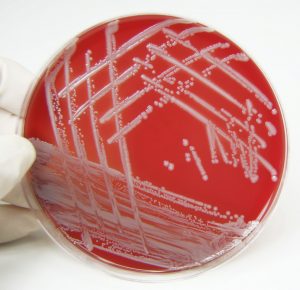
Staph is commonly found in the nose or on the skin, and can lead to infections. The researchers exposed mice to low doses of a protein found in staph and found that the mice developed a lupus-like illness with kidney disease and autoantibodies commonly found in lupus patients.
Advertisement
Coauthor Vaidehi Chowdhary said, “We think this protein could be an important clue to what may cause or exacerbate lupus in certain genetically predisposed patients. Our hope is to confirm these findings in lupus patients and hopefully prevent flares.”
Researchers also question whether treating patients for staph could prevent lupus. Lupus is an autoimmune disorder where the immune system attacks the joints. Lupus is difficult to diagnose, because it can mimic many other disorders, as well as it can affect all parts of the body. It is difficult to determine the cause of lupus, just like in many other autoimmune diseases, but the study results shed light onto at least one possible cause.
In the mice models, the animals were given a staph protein, which is activated by certain white blood cells to set off an inflammatory response that mirrors lupus. In studies conducted on humans, the results confirmed that chronic exposure to staph has contributed to a diagnosis of lupus.
Infections may be fatal for lupus patients
An alternative study explored that opportunistic infections (OIs) may be fatal for lupus patients. Although not common – only affecting nearly one-third of patients – they are quite serious and even fatal. Unfortunately, diagnosing OIs can be difficult, and these infections are often overlooked, as symptoms may resemble lupus flares.
OIs may be caused by immunosuppressant therapy and abnormalities in the immune system. Common bacteria, which lead to OIs in lupus patients, are Escherichia coli, Staphylococcus aureus, Mycobacterium tuberculosis, and Streptococcus pneumoniae.
Aside from being threatening to lupus patients, OIs may onset the condition in individuals without lupus. The authors of the study noted, “Dysregulation of miRNAs due to viral infections, such as EBV [Epstein-Barr virus] or HCV [hepatitis C virus], may promote the development of autoimmunity through their association with components of the RNAi [RNA interference] pathway.” The researchers found 16 microRNAs in lupus patients compared to control ones.
The researchers do note that some infections like malaria and parasitic infections may protect individuals from lupus.
If you have lupus, it is important that you protect yourself from illness and infection, as it can be quite severe. On the other hand, if you don’t have lupus, you can take preventative measures one step further and protect yourself from developing lupus too.
Related Reading:
Metabolic syndrome in lupus affecting women prevented by antimalarial drug
Metabolic syndrome in lupus affecting women can be prevented by antimalarial drug. A recent study uncovered that an antimalarial drug could be effective in preventing metabolic syndrome in women with lupus. Metabolic syndrome is classified by the National Heart, Lung and Blood Institute as, “the name for a group of risk factors that raises your risk for heart disease and other health problems, such as diabetes and stroke.” Continue reading…
Advertisement
Lupus affects lungs, leads to pleuritis, pneumonitis and pulmonary hypertension
Lupus is an autoimmune disease that often impacts the lungs, and research shows pulmonary complications with this disease can lead to pleuritis, pneumonitis, and pulmonary hypertension. When a person has a lung infection, it usually affects their airway and lung tissue, but with lupus it seems that it can impact all compartments of the lungs and include pleuritis, which is inflammation of the linings around the lung, as well as pulmonary hypertension (high blood pressure that occurs in the arteries in the lungs). Continue reading…
Sources:
http://www.sciencedaily.com/releases/2012/08/120808142001.htm
http://www.medscape.org/viewarticle/767113
